Silicosis
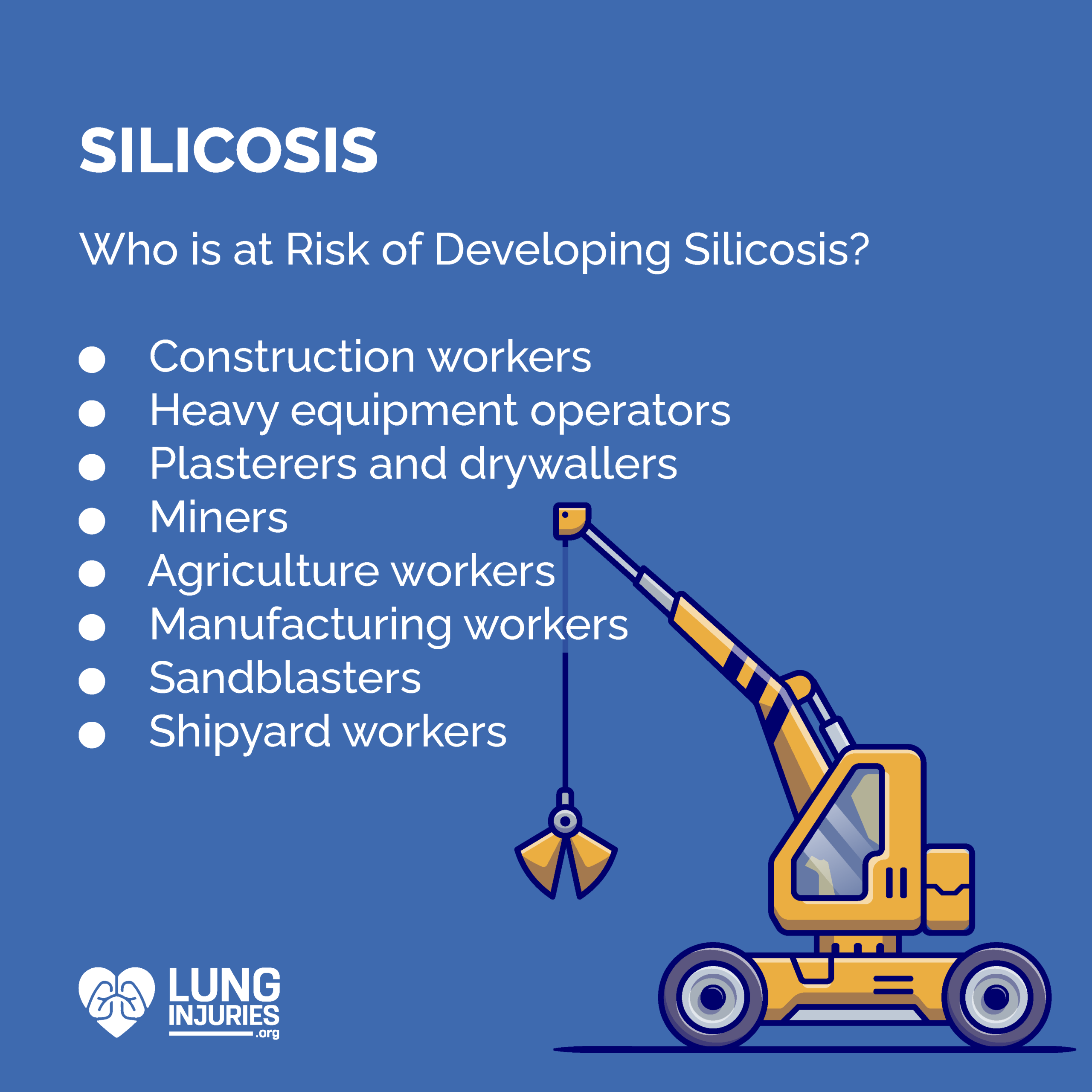
Each year, around 380,000 Canadian workers are occupationally exposed to crystalline silica. Each of these individuals – 93% of which are male – are at risk for developing silicosis.
What is Silicosis?
Silicosis is a lung disease that develops when someone inhales crystalline silica dust. The tiny particles enter the lungs and are difficult to exhale back out. Instead, they can attach themselves to the soft, moist tissues in the lungs. The body then has a response to the foreign particles, which causes:
- Inflammation
- Nodules
- Fluid buildup
Over time, silicosis can develop into a serious lung disease. Silica dust causes an immunologic response once inhaled that causes cell death, inflammation and uncontrolled spread. There is currently no cure for silicosis, and it is a progressive disease. That means that, over time, the disease will only continue to get worse, especially without adequate treatment.
There are three types of silicosis:
- Acute: Acute silicosis can develop only a few months after exposure, but can take up to two years for symptoms to become apparent. Most often, acute cases are the result of exposure to an extremely high concentration of silica dust.
- Chronic: Chronic silicosis is the most common type of the disease. Symptoms generally develop 15-20 years after exposure to silica dust. Most often, chronic cases are the result of low or moderate exposure to silica dust over an extended period of time. Because symptoms often do not appear until years or even decades later, patients often experience lung damage by the time they realize they are sick.
- Accelerated: Accelerated silicosis develops more quickly than chronic. Generally, it is diagnosed 5-10 years after exposure to high concentrations of silica dust.
The type of silicosis you have will impact your symptoms and treatment plan. If you have a history of working around silica dust, talk to your doctor about the possibility of silicosis. There are well-documented epidemics involving silicosis, including one in the 1930’s in West Virginia, USA.
Symptoms
People with silicosis experience a variety of symptoms. Nodules in the lungs can cause breathing problems and a variety of uncomfortable or painful symptoms. Sometimes, nodules will grow into fibroids, which can also damage the lungs and cause more extensive symptoms. Most often, people with silicosis experience the following symptoms based on the type of disease. Many of these symptoms are similar to that of lung cancer or adenocarcinoma. Symptoms may include:
Symptoms of acute silicosis:
- Shortness of breath
- Cough
- Weakness
- Fever
- Weight loss
Symptoms of Chronic Silicosis:
- Shortness of breath
- Fatigue
- Chest pain
- Poor oxygen/carbon dioxide exchange
- Respiratory failure
Symptoms of Accelerated Silicosis:
- Severe shortness of breath
- Weakness
- Weight loss
How is Silicosis Diagnosed?
Diagnosing silicosis begins with a thorough review of your medical and work history, along with a physical examination. From there, your doctor may order a series of laboratory or imaging tests. These tests may include:
- X-Ray: A chest x-ray will identify nodules or scarring.
- Computerized Tomography (CT): A CT scan is a combination of x-ray images that allows doctors to view cross-sections and different angles of the body.
- Bronchoscopy: Doctors insert a long tube into your lungs. There is a camera on the end of the tube that allows them to see the inside of your lungs and assess if there are tumors, fluid or other damage.
- Biopsy: If the doctor sees something abnormal, he or she can take a sample of the tissue to examine it under a microscope. This can be done during a bronchoscopy, or externally using a long thin needle inserted through the skin on your chest.
- Sputum Tests: If you are coughing and have phlegm, your doctor may collect a sample to test in the lab. These tests can tell if there are viruses, fungus, bacteria or the presence of diseases like silicosis.
Your healthcare team will carefully review the results of all of these tests and then will make a diagnosis.
Treatment
There is no cure for silicosis, and treatment options will depend on the severity of the disease and your overall health. The first method of treating your symptoms will be to remove the source of silica dust exposure from your life. Next, if you smoke, your doctor will advise you to quit.
As for treating the disease itself, treatment options are primarily aimed at easing symptoms, slowing down disease progression and maximizing lung function. Some of the treatment methods your healthcare team may recommend include:
- Bronchodilators to relax the airways and reduce inflammation. This can help you breathe more easily.
- Supplemental oxygen, or oxygen therapy, can help get more air into your lungs, and subsequently to the rest of your body.
- Pulmonary rehabilitation can help you manage your symptoms and improve your overall lung function and health.
- In severe cases, your doctor may recommend you speak with a surgeon about a lung transplant.
In addition to these treatment options, your healthcare team will also advise you to maintain a healthy lifestyle. You should stay as active as you can, eat a healthy diet, and avoid smoking or secondhand smoke.
People with silicosis are more at risk for disease like tuberculosis and pneumonia, so you should be mindful of any changes in your symptoms.
Prognosis
Because there is no “cure” for silicosis, people with the disease may reasonably be frightened by the prospect of a long-term disease. However, treatment options can slow down progression and ease symptoms, which can improve overall quality of life and help you live as normal a life as possible. The best way to improve your prognosis is to follow your doctor’s advice every step of the way. Understand the cause of your lung injury and what you can do to improve your symptoms. Stay away from dust, toxins and smoke, and do your best to stay active and healthy. Ultimately, your prognosis will depend on your health and lifestyle, the progression of your disease and how well you respond to treatment.
Sources:
- https://www.ccohs.ca/oshanswers/diseases/silicosis.html
- https://www.constructioncanada.net/construction-and-silicosis-what-you-need-to-know/
- https://www.wsib.ca/sites/default/files/2019-03/0616a_silicosis.pdf
- https://www.thesafetymag.com/ca/archived/crystalline-silica-exposure-in-canada/192391
- https://www.silicosishelp.com/silicosis/what-is-silicosis/

